Vitreous Haemorrhage: Symptoms, Causes, and Prognosis
20 Jun 2025
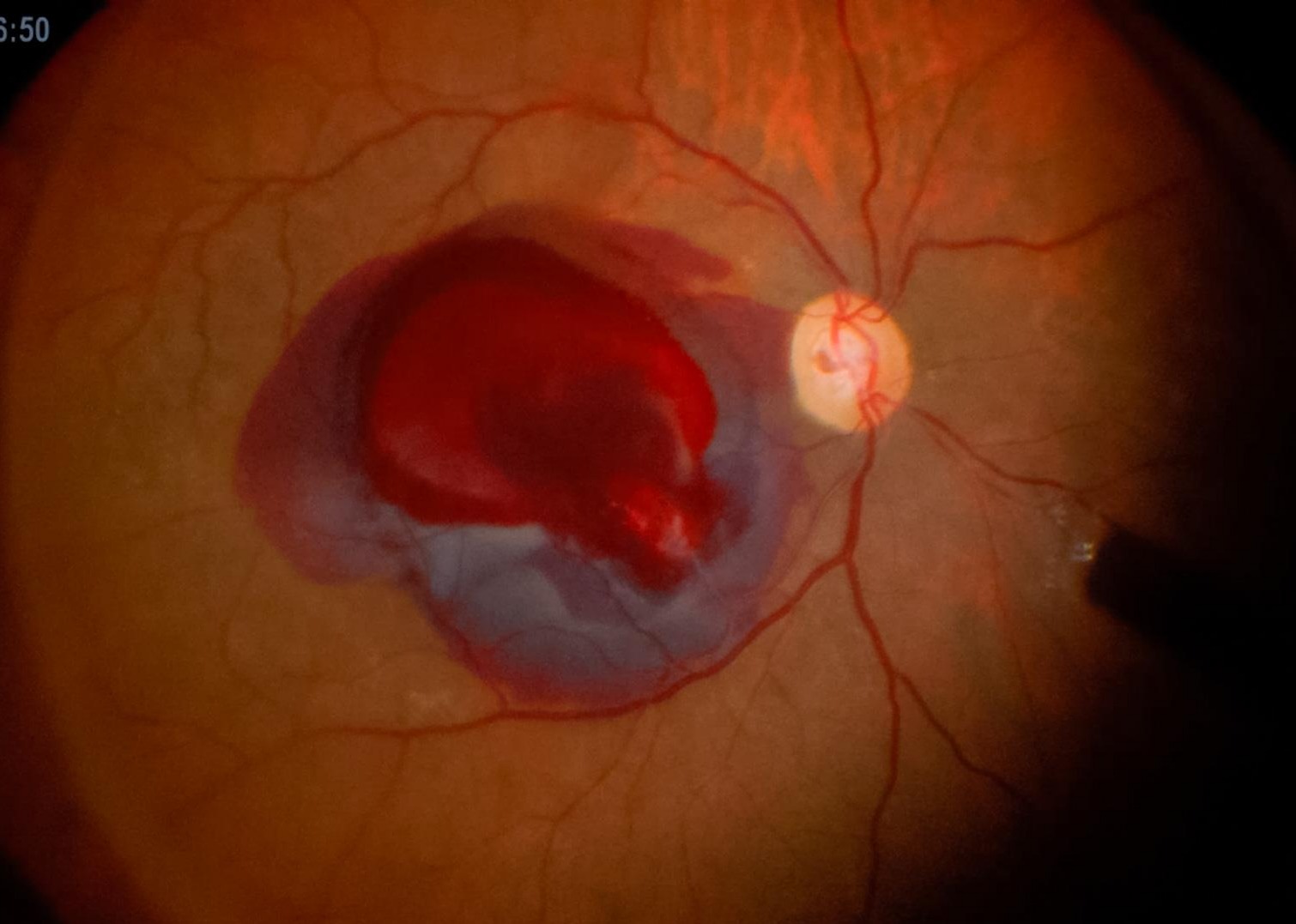
Vitreous haemorrhage occurs when blood leaks into the clear, gel-like substance (vitreous) that fills the space between the lens and the retina at the back of the eye. This blood can block light from reaching the retina, causing sudden visual symptoms like floaters, blurry vision, or even a curtain-like shadow. It’s not painful, but it can be alarming — and in some cases, a sign of serious underlying eye disease.
At DS Eye Surgeon, based at Edgbaston Eye Consultants in Birmingham, we offer expert diagnosis of vitreous haemorrhage — particularly when caused by conditions like diabetic eye disease. While we don’t provide surgical treatment for all causes, we’re often the first step in identifying what’s happening and whether urgent referral is needed.
Overview
Vitreous haemorrhage is bleeding into the vitreous – the clear, gel-like substance that fills the back of the eye. Under normal conditions, the vitreous is transparent, allowing light to pass freely through to the retina, where visual information is processed. However, when blood leaks into this space, it scatters and blocks light, causing visual disturbances such as floaters, haziness, or sudden vision loss.
This condition is usually painless but can be alarming, especially if it occurs suddenly. Many patients describe a “fog,” “cobwebs,” or “red floaters” drifting across their vision. While it often affects only one eye at a time, the impact on daily life can be significant.
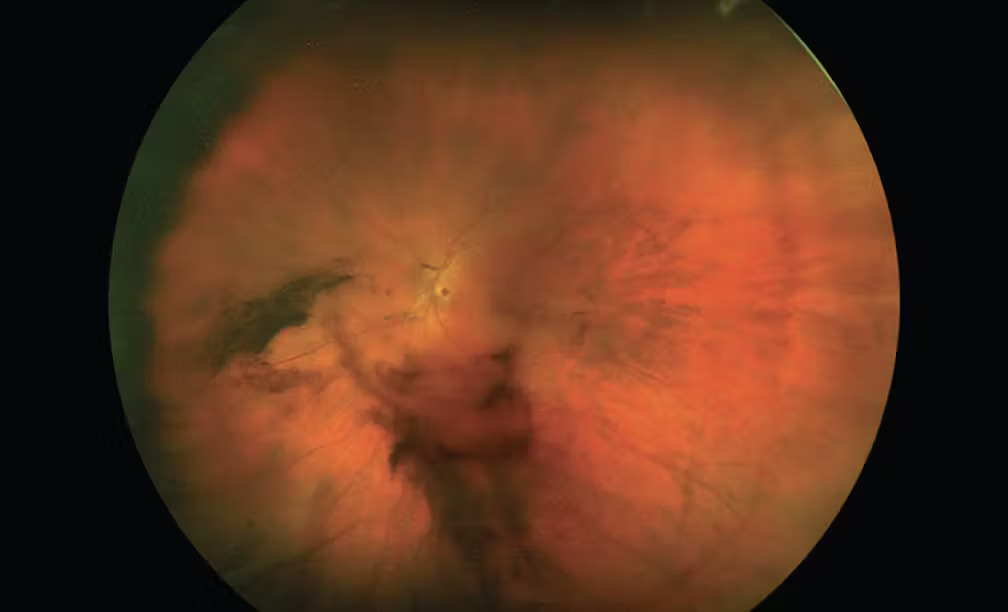
Vitreous haemorrhage is not a disease in itself, but rather a sign of an underlying problem. It most commonly results from abnormal or damaged blood vessels on the retina. These vessels may bleed due to diabetic eye disease (especially proliferative diabetic retinopathy), trauma, or a sudden tear in the retina during a posterior vitreous detachment (a common age-related event). In rare cases, it may result from less common conditions like retinal vein occlusion, ocular tumours, or blood disorders.
This is not a rare condition. It is one of the most common causes of acute vision loss seen in ophthalmology, with studies showing an incidence of around 7 per 100,000 people per year. At DS Eye Surgeon, we frequently diagnose vitreous haemorrhages in patients from across Birmingham, often due to diabetic retinopathy — a condition that I specialise in managing.
The severity of symptoms can range from mild floaters to near-total loss of vision, depending on how much blood enters the vitreous cavity. In some cases, the haemorrhage may be so dense that the retina cannot be visualised properly, requiring follow-up scans or surgical assessment.
Even when symptoms feel dramatic, the key is to understand that vitreous haemorrhage is a sign that should prompt a full dilated eye examination. While some cases resolve on their own, others may point to retinal tears or significant disease that require urgent treatment.
In short: if you’ve noticed sudden floaters or hazy vision, especially if you’re diabetic or over 50, a vitreous haemorrhage could be the cause — and early diagnosis is essential.
Is vitreous haemorrhage serious?
In some cases, a vitreous haemorrhage can be harmless and resolve on its own. But in others, it’s a warning sign of something more serious — especially if it’s caused by:
- A retinal tear or detachment
- Advanced diabetic retinopathy
- Abnormal blood vessels growing in the retina (neovascularisation) secondary to retinal vein occlusion or other cause
These can threaten permanent vision loss if not treated promptly. That’s why any sudden onset of floaters, flashes, or loss of vision should be assessed urgently.
Key symptoms of vitreous haemorrhage:
- A sudden shower of black dots or floaters
- Cloudy or hazy vision
- A red tinge or dark shadow in vision
- Flashes of light
- Difficulty reading or recognising faces
Some people describe it as “looking through a fog”.
At our Birmingham eye clinic, we regularly assess these symptoms using dilated retinal examination and high-resolution OCT scans. If we detect a tear, we’ll urgently refer you to a vitreoretinal surgeon for emergency treatment. If it’s caused by diabetic retinopathy, we can often begin treatment directly in clinic.
What is the treatment for vitreous haemorrhage?
1. Observation
For small bleeds not affecting the central vision, the best course may be to wait. The eye slowly absorbs the blood over weeks to months, especially if the source of bleeding has stopped.
You may be advised to:
- Rest and keep your head upright
- Avoid strenuous activity or lifting
- Return for follow-up eye exams
2. Laser treatment or injections
If the cause is proliferative diabetic retinopathy (PDR), you may need:
- Pan-retinal photocoagulation (laser therapy) to stop abnormal blood vessels
- Anti-VEGF injections into the eye to reduce bleeding and prevent further damage
We provide both of these treatments in-house for appropriate cases.
3. Vitrectomy surgery
If the haemorrhage is severe, persistent, or linked to a retinal detachment, surgery may be required. In this procedure, a vitreoretinal surgeon removes the blood-filled vitreous and replaces it with a clear solution.
At DS Eye Surgeon, we do not perform vitrectomy, but we work closely with a vitreoretinal surgeon for prompt referral and ongoing care coordination.

How long does it take for vitreous haemorrhage to resolve?
This varies depending on the size of the bleed and the underlying cause.
- Small haemorrhages can start to improve within a few days to weeks
- Larger bleeds may take 2 to 4 month or longer to clear
- In some cases, if the blood does not clear or recurs, surgery may be needed
Keeping your head upright helps the blood settle at the bottom of the eye, out of the visual axis. Some people report sudden improvement after a few weeks, while others may experience lingering floaters or haziness for months.
During this time, we monitor progress with repeat retinal scans and fundus checks.
What is the prognosis for vitreous haemorrhage?
The long-term outcome depends on:
- The underlying cause
- The speed of diagnosis and treatment
- The presence of retinal damage
Good prognosis
- If caused by a posterior vitreous detachment (PVD) with no retinal tear, many people make a full recovery without lasting damage.
Cautious prognosis
- If due to diabetic retinopathy, there may be long-term damage or risk of re-bleeding if diabetes is not controlled.
Poorer prognosis
- If a retinal detachment or long-standing PDR is involved, there’s a higher risk of permanent vision loss.
That’s why prompt diagnosis is crucial. At DS Eye Surgeon in Birmingham, we perform dilated funduscopy to quickly identify the cause and start appropriate treatment or referral.
Causes of vitreous haemorrhage
Causes of vitreous haemorrhage (common in private practice)
- Diabetic retinopathy: Abnormal new blood vessels grow and bleed
- Posterior vitreous detachment (PVD): Normal ageing changes that sometimes pull on the retina
- Retinal tear or detachment
- Trauma (e.g. sports injuries or falls)
- Blocked retinal vein (retinal vein occlusion)
As a retinal specialist with expertise in diabetic eye disease, I often see vitreous haemorrhage in patients with poorly controlled or long-standing diabetes. In these cases, early laser and injection therapy can help stabilise vision and prevent further bleeding.
Do I need surgery for vitreous haemorrhage?
Not always — many cases of vitreous haemorrhage do not require surgery and can be safely monitored, especially if the bleed is mild and the underlying cause is stable. However, in some situations, surgery (called vitrectomy) may be recommended to restore vision or to treat the cause of the bleeding.
When observation is appropriate
In many cases — especially if the bleed is partial and the retina can still be visualised — your eye specialist may recommend watchful waiting. Over time (weeks to months), the blood can naturally settle or be reabsorbed by the body. During this period, we monitor closely to ensure no progression or underlying retinal detachment is missed.
Observation is often chosen when:
-
The haemorrhage is mild to moderate
-
There is no retinal tear or detachment
-
The cause (e.g. diabetic retinopathy) is being treated medically
-
You are not in urgent need of visual recovery (e.g. not relying on that eye for driving or work)
When surgery may be needed
A vitrectomy is a surgical procedure where the blood-filled vitreous is removed and replaced with a clear fluid, allowing light to reach the retina again. This may be considered when:
-
The haemorrhage is dense or longstanding, and vision has not improved over several weeks
-
The retina cannot be visualised, making it impossible to rule out a retinal tear or detachment
-
There are recurrent bleeds that impair recovery
-
You rely heavily on the affected eye (e.g. the fellow eye has poor vision)
-
There is tractional retinal detachment, often seen in advanced diabetic retinopathy
Understanding the risks
Vitrectomy is generally safe in experienced hands, but as with any surgery, there are potential risks. These include cataract progression, retinal tears or detachment, infection, and raised intraocular pressure. Therefore, surgery is usually reserved for cases where the benefit outweighs the risk — for example, where vision is severely affected and unlikely to recover with observation alone.
At DS Eye Surgeon in Birmingham, we do not perform surgery on vitreous haemorrhage cases directly — but we can diagnose the cause, assess severity, and refer you appropriately if surgery is needed. We also manage many cases of diabetic eye disease, which is a leading cause of bleeding into the vitreous.
If you’ve experienced a sudden loss of vision, the most important step is to have a dilated fundus examination to determine whether surgery is needed — and if not, how best to monitor or treat the condition medically.
Who should you see in Birmingham?
If you’ve had a sudden change in vision and suspect a vitreous haemorrhage, your options are:
- Emergency referral to BMEC casualty (for retinal tears, detachment or dense bleeds with no fundal view)
- Consultant-led private clinic (like DS Eye Surgeon) for:
- Same-day dilated retinal exams
- OCT imaging to assess the macula and vitreous
- Diabetic retinopathy treatment (laser/injections)
- Advice on next steps, referrals and monitoring
Our Birmingham clinic is located at Edgbaston Eye Consultants, 22 George Road, B15 1PJ, walking distance from Fiveways rail station and bus stop.
Frequently Asked Questions
- Is vitreous haemorrhage an emergency? It needs urgent review because one of the causes is acutely sight-threatening— especially if your vision suddenly drops or you see flashing lights or shadows. You need an urgent eye exam to rule out a retinal tear.
- Can vitreous haemorrhage go away on its own? Yes, small bleeds often clear without treatment over weeks or months. But the underlying cause must still be checked and treated.
- Will my vision return to normal? In many cases, yes — especially if no permanent retinal damage occurred. But floaters or minor haze may persist long-term.
